Blog
*The views expressed here are our own.

Completing 3-4 weeks of physical rehabilitation before undergoing ACL (anterior cruciate ligament) surgery can be a game-changer in recovery and long-term knee health. Many patients want to get surgery over with, but pre-surgical rehab offers several advantages that can lead to better outcomes, quicker recovery, and reduced post-operative complications. Here’s a closer look at why those few weeks of prehabilitation (or “prehab”) are essential and the three primary benefits it offers. 1. Restoring Range of Motion while Reducing Swelling One of the main goals of pre-surgery rehab is to restore as much range of motion as possible and reduce swelling in the knee. An injured ACL often leads to inflammation and restricted movement, which, if left unaddressed, can complicate surgery and prolong recovery time. Why is range of motion important? When the knee is swollen and stiff, it’s challenging to move the joint through its full range. This stiffness can cause problems both during surgery and afterward, as surgeons may need to work around restricted tissues. Regaining flexibility prior to surgery makes it easier for the surgeon to operate and allows for a smoother post-operative healing process. After surgery, achieving full range of motion can be challenging, especially if the knee was stiff before surgery. Prehab helps patients get used to moving the joint and prepares it to regain full motion after the procedure. How does reducing swelling help? Swelling can increase discomfort, and a swollen knee is typically harder for surgeons to operate on. Reducing swelling ahead of time not only makes surgery easier, but it also lessens post-surgical pain. Prehab helps by using modalities such as ice, compression, and low-impact exercises to gradually reduce inflammation and optimize the knee for surgery. Less swelling at the time of surgery also translates to a quicker post-op recovery, as the body has less residual inflammation to clear. 2. Building Girth in Supporting Muscles Another crucial benefit of prehab is strengthening the muscles around the knee, particularly the quadriceps, hamstrings, and gluteal muscles. These muscle groups play a key role in knee stability and movement. Strengthening them before surgery can have a significant impact on post-operative outcomes. The importance of quadriceps strength One of the biggest challenges after ACL surgery is regaining quadriceps strength, as the quadriceps often become weak due to injury, swelling, and limited activity. Strong quadriceps help stabilize the knee and improve joint control, which is vital for successful recovery. If the quadriceps are strengthened before surgery, patients often find it easier to activate them afterward. This leads to quicker gains in strength and functionality during the early stages of post-operative rehab. Enhancing joint stability By focusing on other stabilizing muscles such as the hamstrings and glutes, patients can improve overall joint stability. This muscular support is particularly important because an ACL injury leaves the knee more susceptible to further injuries and instability. Strengthening these muscles reduces this risk, making the knee more resilient and better prepared for the stresses of surgery and the demands of post-operative rehabilitation. With strong supporting muscles, patients are more likely to avoid the compensatory movement patterns that can lead to imbalances and future injuries. 3. Improved Mental Preparedness and Confidence Recovering from an ACL injury can be mentally taxing, and the thought of surgery often adds more stress and anxiety. Prehab helps address these mental challenges by building a routine, setting realistic goals, and fostering a positive mindset. Why mental preparedness matters Undergoing surgery can be daunting, and it’s common for patients to feel a loss of control over their bodies. Prehab provides an opportunity to take charge of recovery, actively working toward the best outcome rather than passively waiting for surgery. This active role can reduce anxiety, increase motivation, and boost overall mental preparedness, helping patients feel more in control of their health. Boosting confidence through movement Being able to move the injured knee through controlled exercises during prehab can boost confidence significantly. Patients may feel reassured that their knee is stronger and more capable than they initially thought, which can ease anxiety about the post-operative rehabilitation process. This confidence is critical, as post-operative recovery requires patience and dedication, and a positive mindset can accelerate this journey. When patients enter surgery knowing they’ve already improved their knee’s strength and mobility, they’re often more motivated to stick to their rehab plan and achieve successful outcomes. In Summary While it may seem tempting to schedule surgery as soon as possible, completing 3-4 weeks of pre-surgical rehabilitation can offer significant benefits that are well worth the time investment. By restoring range of motion, reducing swelling, strengthening key muscle groups, and preparing mentally, patients can set the stage for a smoother surgery, faster recovery, and, ultimately, a more successful return to their active lives.
Concussions are more common in youth than we often realize, affecting children and adolescents who play sports, participate in recreational activities, or even just navigate daily life. While physical restrictions have traditionally been emphasized after a concussion, an equally important aspect of recovery that’s often overlooked are cognitive restrictions and a carefully structured return-to-learn progression. Research and clinical experience show that a structured return to school and learning activities not only aids in a child’s recovery but also reduces the long-term impacts of the concussion. In my practice, all children and adolescents who have a diagnosed concussion receive a return to learn program that is communicated to teachers, coaches and other administrative personnel. In this post, we’ll explore why a gradual return-to-learn progression is essential for young people recovering from a concussion and how it can make a significant difference in their long-term health and academic success. Understanding the Impact of Concussion on the Developing Brain A concussion, or mild traumatic brain injury (mTBI), affects brain function by disrupting neural connections and altering the way the brain communicates with itself and the body. For children and adolescents, whose brains are still developing, the effects of a concussion can be more pronounced and longer-lasting than in adults. The symptoms—ranging from headaches and dizziness to cognitive challenges like poor concentration and memory problems—can interfere significantly with daily activities, particularly with learning. The developing brain is highly plastic and adaptable, which makes it resilient but also vulnerable. When a child or adolescent returns to learning too quickly without allowing the brain to heal, they risk prolonging symptoms, slowing recovery, and, in some cases, worsening outcomes. A structured, phased approach to resuming cognitive activities allows the brain to gradually rebuild its resilience and functionality without undue strain. What is a Return-to-Learn Progression? A return-to-learn progression is a staged approach that helps students reintegrate into academic settings after a concussion in a way that aligns with their recovery. Rather than sending them back to school at full capacity, the process involves a series of steps to gradually increase cognitive load. This gradual return allows the student’s brain to adjust at each stage, reducing the risk of symptom recurrence and supporting sustainable recovery. Generally, the return-to-learn process includes the following stages: 1. Initial Period of Cognitive Rest: Initially, students may need total rest from any cognitive demands, including screen time, reading, homework, and even conversations. 2. Light Cognitive Activity: Students can start low-demand cognitive tasks at home, such as brief reading sessions or listening to music, as long as symptoms remain controlled. 3. Partial School Attendance: At this stage, students may attend school for short periods, focusing on core subjects with breaks as needed to avoid symptom exacerbation. 4. Gradual Return to Full Academic Activity: Gradually, students increase attendance and participation until they can tolerate a full day of classes and regular workloads. 5. Resuming Testing and Assessments: Testing and homework resume last, once a student has fully returned to regular academic activities without symptoms. Why a Structured Return-to-Learn is Crucial 1. Prevents Symptom Aggravation Jumping back into a full school day and workload can overstress a recovering brain. The cognitive demands of a typical school day can exacerbate symptoms, especially if students try to “push through” pain, dizziness, or concentration issues. This can lead to a setback in recovery and may prolong symptoms. By returning to learning gradually, students give their brains the necessary time to heal without being overwhelmed by academic tasks. 2. Supports Cognitive Healing The return-to-learn approach acknowledges the role of cognitive rest and rehabilitation. Just as a sprained ankle requires a graduated return to physical activity, the brain requires a similar approach for cognitive tasks. By gradually increasing cognitive demands, students can rebuild stamina and restore brain function step-by-step, reducing the chance of long-term cognitive issues. 3. Reduces Emotional and Social Stress For many students, school is a central part of their social and emotional world. Extended time away or feeling left behind academically can add anxiety, frustration, and a sense of isolation. By structuring a return that accommodates their limitations, students stay connected to their peers and maintain a sense of normalcy, which is vital for mental health and motivation during recovery. 4. Promotes Academic Success Missing days or weeks of school due to concussion can create academic gaps, which are often difficult to catch up on once the student returns. A phased approach prevents the “all-or-nothing” return, where students feel pressure to catch up while still recovering. Teachers and school administrators can work together to adjust assignments and tests to match the student’s current capacity, allowing them to progress without compromising their learning outcomes. 5. Involves Parents, Teachers, and Healthcare Providers in Recovery A return-to-learn progression provides a structured framework that helps parents, teachers, and healthcare providers monitor the student’s progress. Communication and support from these key people ensure that adjustments are made as needed and that any signs of symptom return are promptly addressed. This collaborative approach also ensures that parents and educators are aware of the student's needs and can advocate for adjustments when necessary. The Take Home Message Returning to learn after a concussion is not a “one-size-fits-all” process. Every brain injury is unique, and recovery times vary widely. A structured return-to-learn progression allows children and adolescents to return to school in a safe, supportive way that aligns with their healing process. By recognizing the importance of a phased return, we can help students recover fully, stay connected academically and socially, and set a foundation for lifelong brain health. When parents, teachers, and healthcare providers work together to implement this approach, they support not only the immediate recovery of the child but also their long-term well-being and academic success.

Navigating the healthcare system can be challenging, especially for individuals dealing with concussions or orthopedic injuries. Between managing pain, deciphering treatment options, and scheduling follow-ups, patients often find themselves overwhelmed. Patient navigation services provide essential guidance to help patients make informed decisions and streamline their care journey. These services, increasingly common in many healthcare settings, can improve outcomes by reducing delays in treatment, improving access to resources, and enhancing overall patient satisfaction. Here’s how patient navigation services benefit those with concussions or orthopedic injuries. 1. Streamlining the Path to Diagnosis and Treatment For many patients, the initial steps in treating a concussion or orthopedic injury involve multiple appointments with specialists, diagnostic imaging, and follow-up visits. Without a clear plan, patients might experience delays in receiving the care they need, potentially worsening their condition or prolonging recovery. Patient navigators help coordinate these steps, ensuring that patients receive timely appointments, understand the sequence of care, and avoid unnecessary wait times. They can assist with scheduling, coordinating with various healthcare providers, and even facilitating communication between doctors and patients. This streamlined approach allows patients to begin their treatment faster, reducing the risk of complications and optimizing the recovery timeline. 2. Enhancing Access to Specialized Care Concussions and orthopedic injuries require specific expertise that may not be available in every healthcare setting. For example, concussion care often involves specialists like neurologists, sports medicine doctors, and physical therapists trained in post-concussion rehabilitation. Orthopedic injuries might require orthopedic surgeons, physical therapists, and pain management specialists. Without guidance, patients may struggle to identify and connect with the right specialists, potentially delaying their recovery. Patient navigators have a thorough understanding of the healthcare landscape and can connect patients with appropriate specialists based on their injury and specific needs. By helping patients access specialized care sooner, navigators reduce the likelihood of complications from delayed or ineffective treatments and ensure that patients receive care tailored to their condition. 3. Supporting Patient Education and Self-Management Education is a critical component of recovery, particularly for concussions and orthopedic injuries where patients play a significant role in managing symptoms. Concussion patients, for instance, need to know how to recognize worsening symptoms, practice safe activity levels, and avoid triggers that could exacerbate their injury. Orthopedic patients often need guidance on proper exercise techniques, post-surgery care, and pain management. Patient navigators provide valuable educational resources, explain treatment plans in simple terms, and empower patients to be proactive in their recovery. They may also offer advice on lifestyle modifications, such as proper nutrition, sleep, and stress management, which are essential for healing. This support enhances patients’ ability to manage their own recovery effectively, improving both short- and long-term outcomes. 4. Addressing Barriers to Care and Treatment Adherence For some patients, barriers such as transportation, finances, and work schedules can impede access to necessary care. These obstacles are particularly common in cases of chronic pain, where consistent physical therapy or follow-up appointments are crucial but can be difficult to attend regularly. Patient navigators work closely with patients to identify and address these barriers, often by connecting them with community resources, financial assistance programs, or alternative care options that fit their needs. By proactively addressing these challenges, navigators help patients stay on track with their treatment plans, which is essential for recovery from both concussions and orthopedic injuries. 5. Providing Emotional and Mental Health Support Dealing with a concussion or orthopedic injury can be emotionally taxing. Patients often face stress, anxiety, or frustration related to pain, mobility limitations, and the potential for long-term impact on their daily life. This emotional toll can impact recovery, as stress can interfere with healing and may even discourage patients from adhering to their treatment plans. Patient navigators offer a source of encouragement and understanding, helping to reduce the emotional burden on patients. In some cases, navigators can connect patients with mental health resources, support groups, or counseling services. Having this kind of emotional support can make a significant difference in a patient’s outlook, increasing their resilience and motivation throughout the recovery process. 6. Coordinating Multidisciplinary Care Recovery from a concussion or orthopedic injury often requires a multidisciplinary approach, involving multiple healthcare providers with different areas of expertise. Coordinating care among these providers can be complex and time-consuming, especially when trying to ensure that all aspects of a patient’s treatment are aligned and cohesive. Patient navigators act as a central point of contact, facilitating communication among different specialists to create a well-rounded care plan. By coordinating this multidisciplinary care, they help avoid conflicting recommendations and ensure that each provider is informed of the patient’s progress. This holistic approach allows for a more cohesive treatment experience, reducing redundancies and ensuring that every aspect of a patient’s recovery is addressed. The Impact of Patient Navigation on Recovery and Outcomes Overall, patient navigation services make it easier for individuals with concussions and orthopedic injuries to access timely, specialized, and coordinated care. By helping patients overcome logistical and emotional barriers, providing educational support, and promoting treatment adherence, navigators play a crucial role in enhancing recovery outcomes. Studies have shown that patients who work with navigators often experience shorter recovery times, lower healthcare costs, and higher satisfaction with their care. For healthcare providers, investing in patient navigation services is an effective way to improve patient outcomes and experiences. For patients, navigation services offer a guiding hand through what can often feel like an overwhelming and complicated process, helping them get back to health and regain confidence in their physical abilities.

When we think about movement and exercise, our focus often goes straight to muscles like the glutes, quads, or core. However, there’s a lesser known yet immensely powerful player that underpins efficient, balanced movement: the diaphragm. As the primary muscle of respiration, the diaphragm does much more than help us breathe; it’s also instrumental in stabilizing our core, balancing muscle activation, and supporting proper joint alignment. Understanding the role of the diaphragm in movement can unlock pathways to better physical performance and reduce the risk of injury. What Makes the Diaphragm So Important? The diaphragm is a large, dome-shaped muscle located at the base of the ribcage, separating the thoracic cavity from the abdominal cavity. When we inhale, the diaphragm contracts, pulling downward to create space in the chest cavity, allowing the lungs to fill with air. But breathing is just one of the diaphragm’s essential functions. It also contributes to core stability, muscle relaxation, and joint alignment—all of which are crucial for efficient and balanced movement. Let’s dive into how the diaphragm supports movement in three main ways: relaxing tonic muscles, activating phasic muscles, and assisting with proper joint centration. 1. Diaphragmatic Breathing Relaxes Tonic Muscles Tonic muscles are those that tend to be active at low levels throughout the day to maintain posture and stability. Examples include the upper traps, the pectoralis minor, and the hip flexors. These muscles are prone to becoming overactive and tight, especially if we have poor posture, stress, or inefficient breathing patterns. Diaphragmatic breathing helps to counterbalance this tension. When we engage in slow, deep diaphragmatic breathing, the parasympathetic nervous system—the part of the nervous system responsible for rest and relaxation—becomes more active. This activation has a calming effect on tonic muscles, allowing them to release and relax. It’s a bit like pressing a reset button, helping to counteract the effects of chronic stress and poor posture. By promoting relaxation, diaphragmatic breathing prevents tonic muscles from remaining in a state of constant tension, which can lead to muscle imbalances and restricted movement patterns. 2. Diaphragmatic Breathing Activates Phasic Muscles Phasic muscles are responsible for generating movement. These muscles, such as the glutes, deltoids, and abdominals, are activated during specific activities, such as lifting, walking, or running. Unlike tonic muscles, phasic muscles should only engage when needed and should be allowed to relax when not in use. Diaphragmatic breathing plays a role in activating phasic muscles by creating intra-abdominal pressure (IAP), which stabilizes the core and allows other muscles to engage efficiently. When we breathe deeply with the diaphragm, IAP is created, giving the phasic muscles a strong and stable base from which to work. This process aids in core stability and ensures that muscles like the glutes and deep abdominals are activated properly, supporting movement without overloading the low back or other parts of the body. When phasic muscles are activated appropriately, they do the “heavy lifting” of movement, while the relaxed tonic muscles can provide necessary postural support. This balance between muscle groups contributes to better movement efficiency, as each muscle type is fulfilling its proper role. 3. Diaphragmatic Breathing and Proper Joint Centration Joint centration refers to the optimal alignment of a joint, where it’s centered within the socket and balanced by equal muscle tension around it. Proper joint centration is crucial for efficient movement and injury prevention, as it reduces unnecessary strain on the joint structures. Diaphragmatic breathing assists with joint centration by engaging the deep core muscles, including the transverse abdominis, pelvic floor, and multifidus muscles, which help stabilize and align the spine and pelvis. When the diaphragm contracts during inhalation, it works in concert with these deep muscles to create intra-abdominal pressure, stabilizing the trunk and aligning the joints in the hips, spine, and shoulders. This core stability allows the body to maintain proper joint alignment during movement, preventing excessive wear on the joints. Without diaphragmatic support, the spine and other joints can become misaligned, increasing the risk of compensatory movements and injury. Joint centration facilitated by diaphragmatic breathing thus creates a foundation for fluid, balanced movement. Practical Benefits of Training the Diaphragm 1. Improved Posture Since the diaphragm plays a role in stabilizing the spine, breathing with the diaphragm helps promote better posture. This improved posture reduces tension in the neck, shoulders, and lower back, making it easier to maintain alignment during activities. 2. Increased Core Stability Diaphragmatic breathing engages the core muscles in a way that supports functional stability. With a stable core, movements become more powerful and controlled, reducing the likelihood of injury during exercise or everyday activities. 3. Enhanced Flexibility and Range of Motion Relaxed tonic muscles and engaged phasic muscles contribute to a better balance in flexibility and mobility. Diaphragmatic breathing allows tight muscles to release and facilitates a greater range of motion, improving performance and reducing injury risk. 4. Better Balance and Coordination With the diaphragm’s role in stabilizing the core and centering joints, balance and coordination improve. The body becomes more responsive and resilient to changes in movement, making it easier to perform activities with precision and control. The TLDR The diaphragm is much more than a muscle for breathing—it’s a powerful stabilizer, a relaxation agent, and a key player in efficient movement. Diaphragmatic breathing activates the body’s innate balance between tonic and phasic muscles, encourages proper joint centration, and enhances posture and coordination. By focusing on diaphragmatic breathing, you’re setting the stage for a body that moves with ease, stability, and resilience. Whether you’re aiming for athletic performance or simply looking to move more comfortably in daily life, the diaphragm is the foundation of a balanced and efficient movement system .
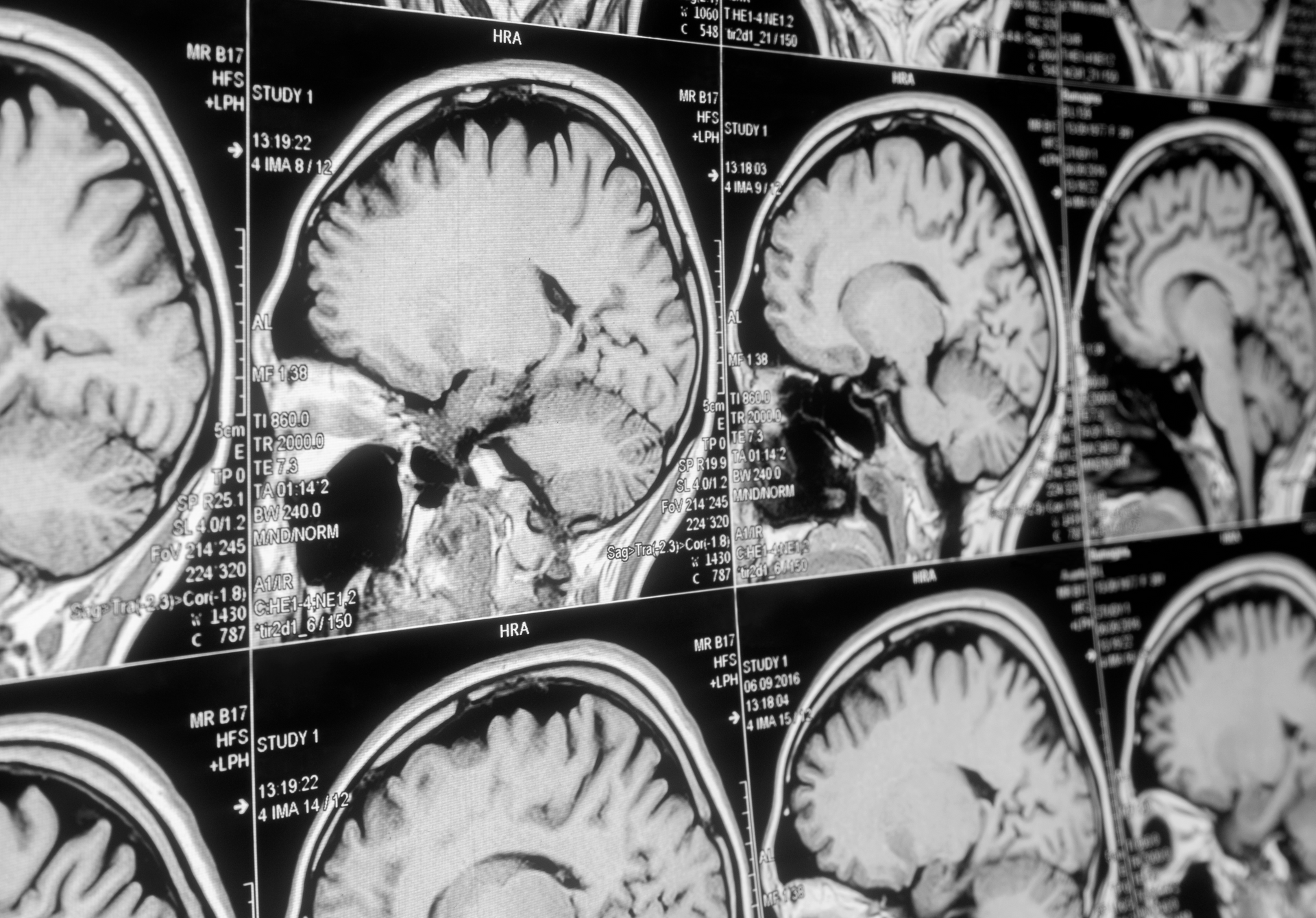
A concussion can be a scary experience, especially when symptoms like dizziness, confusion, or headaches follow an impact to the head. Naturally, many people feel an urge to head to the emergency room (ER) to get checked out. However, for most concussions, the ER isn’t the best place to go. In many cases, it may not provide the right type of assessment or treatment for this type of injury. Here’s why a concussion typically doesn’t warrant a trip to the ER and why seeing a specialist is often the most effective course of action. 1. Concussion Is Typically Not a Life-Threatening Emergency Concussions are a form of mild traumatic brain injury (TBI), but they are usually not life-threatening. While symptoms can be unpleasant and sometimes alarming, they generally do not indicate an immediate medical emergency. In most cases, symptoms are manageable and can be monitored at home or through a visit to a specialist with expertise in concussion. Emergency room visits are often necessary for severe or urgent medical conditions, but unless there are signs of a more serious brain injury, a trip to the ER for a concussion is just a waste of your time and money. 2. ER Physicians Are Not Specialized in Concussion Evaluation ER doctors are highly skilled in handling immediate, life-threatening conditions like trauma, stroke, and heart attacks, but they typically do not specialize in concussion diagnosis and treatment. While ER doctors can perform basic neurological exams, they are not trained to conduct the specific assessments that concussion specialists perform. Concussion injuries are complex and often require a specialized evaluation, which may include targeted diagnostic tools to understand the extent of the injury and guide recovery. Without these specific tools and expertise, an ER visit might result in a very general assessment that overlooks specific concussion related impairments. 3. Concussions Do Not Show in Standard Imaging Many people assume that the ER can confirm a concussion diagnosis with imaging like a CT scan. However, most concussions do not show up on standard imaging tests. Concussions involve microscopic changes in brain function, which do not usually appear on CT or MRI scans unless there is a more severe injury, such as a brain bleed or skull fracture. 4. A Specialist Is Needed for Proper Diagnosis and Treatment A concussion injury requires evaluation and management by a healthcare provider trained in concussions. These providers use specific diagnostic protocols to determine the severity of the injury, track symptoms over time, and assess factors like cognitive function, balance, and visual tracking. Additionally, they can develop a personalized treatment plan tailored to the individual’s recovery. The post-injury management of a concussion is also crucial, and specialists are equipped to provide a structured recovery plan that addresses cognitive rest, physical activity restrictions, and gradual re-introduction to normal activities. Without this type of guided recovery, people may risk returning to normal activities too soon, potentially prolonging their symptoms or even increasing the risk of long-term complications. 5. When an ER Visit *Is* Necessary for a Concussion While most concussions don’t require an ER visit, there are situations where it’s crucial to seek emergency care. If any of the following symptoms are present, immediate medical attention is necessary: - Repeated vomiting - Loss of consciousness - Seizures - Numbness, weakness, or decreased coordination - Slurred speech or difficulty waking up These could indicate a more severe injury, such as a brain bleed, which would require immediate medical intervention. In such cases, the ER can perform imaging and other tests to rule out life-threatening conditions. Finding the Right Care for Concussion If you or someone you know experiences a suspected concussion, consider seeking care from a provider with concussion expertise rather than heading to the ER. The ER is an invaluable resource for life-threatening emergencies, but for most concussion cases, it isn’t the best place for evaluation and care. Concussions require specific expertise to diagnose, monitor, and manage effectively. By seeking a specialist with experience in concussion management, you can ensure a more accurate diagnosis, proper guidance for recovery, and, ultimately, a smoother path to healing.

“First move well, then move often,” a phrase coined by revered physical therapist Gray Cook has become a guiding principle for how I help others maximize their health, avoid injury, and optimize for performance. What does it mean? Before pushing your body through intense or repetitive movements, it’s essential to establish a foundation of proper movement mechanics. This approach not only maximizes physical efficiency but also focuses on the integration of developmental movement principles. At its core, Cook’s philosophy is about respecting the body’s ingrained movement patterns and understanding the clinical implications of how poor body mechanics results in pain and injury. Why Moving Well Matters When people think about fitness, they often picture complex workouts or rigorous training schedules. But no matter the level of ambition or dedication, the basics of proper body movement are paramount. Imagine trying to build a house without a stable foundation. Without proper movement, even the strongest athletes risk experiencing pain, setbacks, and potential injury. Poor movement patterns often originate from modern, sedentary lifestyles, improper training, or simply a lack of body awareness. When these patterns are left unaddressed, they may lead to overuse injuries, muscle imbalances, and chronic pain. This is especially true for people who dive into training without first assessing their current movement quality. Pain, whether acute or chronic, is frequently the result of dysfunctional movement patterns that place excess stress on specific parts of the body. Cook's statement underscores the importance of prioritizing movement quality before quantity. This order helps reduce injury risk, prevent the need for corrective interventions, and support lifelong physical health. The Clinical Model of Regional Interdependence (RI) A useful model I use for understanding the impact of movement on injury risk is the concept of Regional Interdependence (RI). RI is the idea that different areas of the body are interconnected, and an issue in one area can lead to compensatory stress or dysfunction in another. In other words, pain is often not localized; it can originate from, or be influenced by, dysfunction in a seemingly unrelated part of the body. Correcting the underlying dysfunction often leads to resolution of pain or chronic imbalance. Take, for example, a runner who experiences knee pain. While it’s natural to assume the knee is the problem, a deeper look might reveal that the actual issue lies in the pelvis or foot. According to RI, if the pelvis lacks proper stability, the knee might compensate by taking on extra load. Over time, this compensation can lead to knee pain and injury. By examining the whole chain of movement and considering how different body segments interact, we gain insights into the root causes of pain and develop effective interventions. Identifying Movement Dysfunction with RI Regional Interdependence helps clinicians identify and correct potential areas of dysfunction. By focusing on how different body regions interact, we assess a broader range of possible pain origins. Movement assessments like the Functional Movement Screen (FMS) and Selective Functional Movement Assessment (SFMA), developed by Cook himself, focus on evaluating fundamental movement patterns to identify areas of restriction or weakness that could lead to compensatory movement. For example, a common area of dysfunction is the hip joint, which should be highly mobile. If hip mobility is restricted due to a sedentary lifestyle or tight muscles, other parts of the body, such as the lower back or knees, may compensate for this lack of movement, potentially leading to pain or injury in these areas. This compensatory cycle is known as a “movement impairment syndrome” and is commonly seen in the lower back, shoulder, and knee. The purpose of using RI in clinical assessments is to interrupt these compensatory patterns before they result in pain or injury, providing a framework for both injury prevention and treatment. Practical Steps to Move Well and Correct Dysfunction 1. Assess Your Movement A professional assessment with a physical therapist or movement specialist can help you understand your current movement patterns and identify any areas of concern. Tools like the FMS or other movement assessments can reveal where you need to improve flexibility, mobility, or stability. 2. Focus on Mobility and Stability According to the RI model, each joint has specific requirements for either mobility or stability. The ankle, hip, and thoracic spine, for example, typically need greater mobility, while the knee, lumbar spine, and scapulae benefit from stability. Developing this balance between mobility and stability in your joints is key to establishing healthy, pain-free movement patterns. 3. Strengthen Weak Links Many people unknowingly rely on dominant muscle groups to compensate for weaker ones. Once weaknesses or imbalances are identified, targeted exercises can help restore balanced muscle function, reducing the chance of overload in any one area. 4. Gradually Increase Movement Volume Once foundational movement quality is established, it’s safer to increase the intensity or volume of training. This progressive approach helps build resilience in the body without causing undue stress or overloading the system prematurely. 5. Listen to Your Body Persistent pain or discomfort is often the body’s way of signaling an underlying issue. Paying attention to these signals and adjusting movement as needed can prevent minor aches from becoming major injuries. Moving Well for Life Applying Gray Cook’s principle of “first move well, then move often” and the RI model to daily life and fitness routines can be transformative. When individuals prioritize quality of movement over quantity, they cultivate greater resilience, reduce the risk of injury, and enjoy an active lifestyle without unnecessary pain. Cook’s approach, combined with the insights provided by Regional Interdependence, offers a comprehensive pathway to move well, move often, and stay pain-free.